Shortly before I left for holiday, the International Society for Stem Cell Research (ISSCR) issued a policy paper, “Guidelines for the Clinical Translation of Stem Cells,” outlining ethical and scientific considerations for researchers designing translational trials involving stem cells (whether stem cell derived, adult, or embryonic).
Shortly before I left for holiday, the International Society for Stem Cell Research (ISSCR) issued a policy paper, “Guidelines for the Clinical Translation of Stem Cells,” outlining ethical and scientific considerations for researchers designing translational trials involving stem cells (whether stem cell derived, adult, or embryonic).
In my opinion, the document wins the award for most forward thinking and comprehensive statement on the ethics of a translational enterprise. It shows that the stem cell research leadership has closely studied mistakes made by translational researchers in other highly innovative fields. But the guidelines do more than look backwards; they proactively contemplate fairness and justice considerations as well. Here are a few justice-related excerpts:
On responsiveness: “The ISSCR strongly discourages conduct of trials in a foreign country solely to benefit patients in the home country of the sponsoring agency. The test therapy, if approved, should realistically be expected to become available to the population participating in the clinical trial through existing health systems or those developed on a permanent basis in connection with the trial.”
On reasonable availability: “As far as possible, groups or individuals who participate in clinical stem cell research should be in a position to benefit from the results of this research.”
On diversity: “Stem cell collections with genetically diverse sources of cell lines should be established”
On access and licensing: “Commercial companies, subject to their financial capability, should offer affordable therapeutic interventions to persons living in resource-poor countries who would otherwise be wholly excluded from benefiting from that stem cell-based therapy. Academic and other institutions that are licensing stem cell therapeutics and diagnostic inventions should incorporate this requirement in their intellectual property license”
On review: “Regulatory and oversight agencies (local, national, and international) must explicitly include the consideration of social justice principles into their evaluations.”
On trial participation: “… the sponsor and principal investigator have an ethical responsibility to make good faith, reasonable efforts whenever possible to secure sufficient funding so that no person who meets eligibility criteria is prevented from being considered for enrollment because of his or her inability to cover the costs of the experimental treatment.”
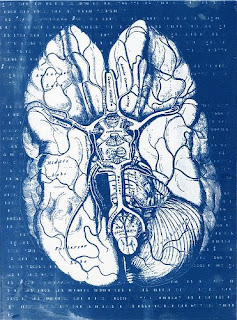
In upcoming posts, I will comment on other aspects of the ISSCR guidelines. (photo credit: Helen K, Stems, 2008)
 Approving new drugs is a risky business. Despite best efforts (and frankly, some less than best efforts), newly approved drugs frequently turn out to have unexpected toxicities. One example is unexpected heart toxicity associated with the use of the common pain-killers like rofecoxib (i.e. Vioxx). Another is the surprising heart toxicity associated with the wonder drug for AML (a type of leukemia), imatinib mesylate (i.e. Gleevec).
Approving new drugs is a risky business. Despite best efforts (and frankly, some less than best efforts), newly approved drugs frequently turn out to have unexpected toxicities. One example is unexpected heart toxicity associated with the use of the common pain-killers like rofecoxib (i.e. Vioxx). Another is the surprising heart toxicity associated with the wonder drug for AML (a type of leukemia), imatinib mesylate (i.e. Gleevec).