High attrition rates in drug development bedevil drug developers, ethicists, health care professionals, and patients alike. Increasingly, many commentators are suggesting the attrition problem partly relates to prevalent methodological flaws in the conduct and reporting of preclinical studies.
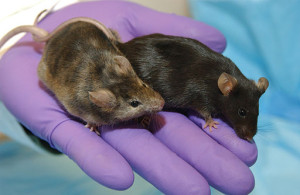
Preclinical efficacy studies involve administering a putative drug to animals (usually mice or rats) that model the disease experienced by humans. The outcome sought in these laboratory experiments is efficacy, making them analogous to Phase 2 or 3 clinical trials.
However, that’s where the similarities end. Unlike trials, preclinical efficacy studies employ a limited repertoire of methodological practices aimed at reducing threats to clinical generalization. These quality-control measures, including randomization, blinding and the performance of a power calculation, are standard in the clinical realm.
This mismatch in scientific rigor hasn’t gone unnoticed, and numerous commentators have urged better design and reporting of preclinical studies. With this in mind, the STREAM research group sought to systematize current initiatives aimed at improving the conduct of preclinical studies. The results of this effort are reported in the July issue of PLoS Medicine.
In brief, we identified 26 guideline documents, extracted their recommendations, and classified each according to the particular validity type – internal, construct, or external – that the recommendation was aimed at addressing. We also identified practices that were most commonly recommended, and used these to create a STREAM checklist for designing and reviewing preclinical studies.
We found that guidelines mainly focused on practices aimed at shoring up internal validity and, to a lesser extent, construct validity. Relatively few guidelines addressed threats to external validity. Additionally, we noted a preponderance of guidance on preclinical neurological and cerebrovascular research; oddly, none addressed cancer drug development, an area with perhaps the highest rate of attrition.
So what’s next? We believe the consensus recommendations identified in our review provide a starting point for developing preclinical guidelines in realms like cancer drug development. We also think our paper identifies some gaps in the guidance literature – for example, a relative paucity of guidelines on the conduct of preclinical systematic reviews. Finally, we suggest our checklist may be helpful for investigators, IRB members, and funding bodies charged with designing, executing, and evaluating preclinical evidence.
Commentaries and lay accounts of our findings can be found in PLoS Medicine, CBC News, McGill Newsroom and Genetic Engineering & Biotechnology News.
BibTeX
@Manual{stream2013-300,
title = {Uncaging Validity in Preclinical Research},
journal = {STREAM research},
author = {Valerie Henderson},
address = {Montreal, Canada},
date = 2013,
month = aug,
day = 5,
url = {https://www.translationalethics.com/2013/08/05/uncaging-validity-in-preclinical-research/}
}
MLA
Valerie Henderson. "Uncaging Validity in Preclinical Research" Web blog post. STREAM research. 05 Aug 2013. Web. 22 Oct 2024. <https://www.translationalethics.com/2013/08/05/uncaging-validity-in-preclinical-research/>
APA
Valerie Henderson. (2013, Aug 05). Uncaging Validity in Preclinical Research [Web log post]. Retrieved from https://www.translationalethics.com/2013/08/05/uncaging-validity-in-preclinical-research/